|
Dr. Abou Abdallah and the
staff of the Middle East Center for Fertility and IVF are here to help you.
We are experienced in all aspects of fertility treatment and provide
compassionate support to our patients.
Our
primary goal is to insure patient satisfaction.

|
|
|
Intrauterine Insemination
Intrauterine insemination (IUI) is
often effective in treating couples with mild male factor disease or
ovulatory dysfunction. IUI is also a "first line" treatment for
couples with "poor" cervical mucus or when antisperm antibodies are
present. IUI can also be used in couples with unexplained
infertility, especially when the female is under 35 years of age.
Success rates with IUI are only half those for IVF in similar female
age groups.
Sperm are provided by masturbation,
concentrated and specially prepared (washed) by the andrologist.
This procedure removes any antigens that might cause an allergic
reaction in the female. "Unwashed" sperm must never be used as
serious allergic reactions can result. If the sperm count is low,
concentrating the sample increases the number of sperm/milliliter.
In IUI, Follicle stimulating hormone (FSH),
Clomid, or a combination of the two, is administered to the female
to insure the development of adequate follicles. Human chorionic
gonadotropin is administered to stimulate ovulation 36-38 hours
prior to the insemination.
FSH should only be administered by a
reproductive endocrinologist thoroughly trained in its use as side
effects can result. The number of follicles developing must be
carefully monitored as high order multiple births can result. Most
of the cases of quadruplets and above reported in the media are due
to IUI not IVF. Specialists are trained to minimize this
possibility. Estradiol levels must also be regularly monitored to
guard against a potentially serious side effect known as
hyperstimulation syndrome.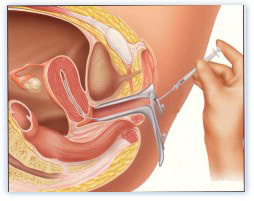
The prepared sperm are placed in a
small catheter and inserted directly into the uterus, thus bypassing
the cervical mucus. This is a painless outpatient procedure that
takes less than five minutes.
Dr. Abou Abdallah has had good success
with IUI .. The advantages of this protocol are that there is less
likelihood of too many follicles developing and the cost is reduced.
If a patient is not pregnant after
three cycles of IUI, the next step is usually in vitro
fertilization.
 top
top
|
Therapeutic Insemination with Donor Sperm
(TID)
TID is the placement of donor sperm directly into the uterus
of the patient.
In cases of
severe male factor infertility, i.e., very low sperm count and/or motility,
or no sperm at all, TID may be indicated. TID may also be used if the male
partner carries a genetic disorder.
Procedure: The procedure is
the same as for IUI, but with the use of donor sperm. Donor sperm are frozen
and stored for 6 months, to enable adequate screening and help prevent
communicable diseases from being transmitted. Frozen donor sperm will be
thawed and processed to isolate the highest quality sperm and then placed
directly into the uterus via a catheter.
 top
top
In Vitro Fertilization is commonly referred to as IVF
There are basically five steps in the IVF
and embryo transfer process which include the following:
-
Monitor and stimulate the development of healthy egg(s) in
the ovaries.
-
Collect the eggs.
-
Secure the sperm.
-
Combine the eggs and sperm together in the laboratory and
provide the appropriate environment for fertilization and early embryo
growth.
-
Transfer embryos into the uterus.
Step 1: Fertility medications
are prescribed to control the timing of the egg ripening and to increase the
chance of collecting multiple eggs during one of the woman's cycles. This is
often referred to as ovulation induction. Multiple eggs are desired
because some eggs will not develop or fertilize after retrieval. Egg
development is monitored using ultrasound to examine the ovaries and urine
or blood test samples to check hormone levels.
Step 2: Your eggs are
retrieved through a minor surgical procedure which uses ultrasound imaging
to guide a hollow needle through the pelvic cavity. Sedation and local
anesthesia are provided to remove any discomfort that you might experience.
The eggs are removed from the ovaries using the hollow needle, which is
called follicular aspiration. Some women may experience cramping on
the day of retrieval, which usually subsides the following day; however, a
feeling of fullness or pressure may last for several weeks following the
procedure.
Step 3: Sperm, usually
obtained by ejaculation is prepared for combining with the eggs.
Step 4: In a process called
insemination, the sperm and eggs are placed in incubators located
in the laboratory which enables fertilization to occur. In some cases where
fertilization is suspected to be low, intracytoplasmic sperm injection
(ICSI) may be used. Through this procedure, a single sperm is injected
directly into the egg in an attempt to achieve fertilization. The eggs are
monitored to confirm that fertilization and cell division are taking place.
Once this occurs, the fertilized eggs are considered embryos.
Step 5: The embryos are
usually transferred into the woman's uterus anywhere from one to six days
later, but most commonly it occurs between two to three days following egg
retrieval. At this point, the fertilized egg has divided to become a
two-to-four cell embryo. The transfer process involves a speculum which is
inserted into the vagina to expose the cervix. A predetermined number of
embryos are suspended in fluid and gently placed through a catheter into the
womb. This process is often guided by ultrasound. The procedure is usually
painless, but some women experience mild cramping.
These steps are followed by rest and watching for early
pregnancy symptoms. A blood test and potentially an ultrasound will be used
to determine if implantation and pregnancy has occurred.
 top
top
Intracytoplasmic Sperm Injection (ICSI)
ICSI is a procedure used in conjunction with
IVF to help couples with moderate to severe male factor infertility,
unexplained infertility, failed fertilization, and other conditions. ICSI
involves the injection of a single sperm directly into an egg after
withdrawal from the ovarian follicles in a stimulated IVF cycle. Before
ICSI, the only option for couples with moderate to severe male factor
infertility was to use donor sperm.
If the male produces enough viable sperm in his ejaculate, it
is collected by masturbation. ICSI also makes it possible for men with
little or no sperm in their ejaculates to father children. Procedures such
as testicular sperm aspiration (TESA) and microscopic epididymal sperm
aspiration (MESA) allow retrieval of sperm directly from the reproductive
tract. Sperm are extracted from the testicles in TESA and from the
epididymis (numerous small tubules within the scrotum) in MESA.
The sperm are specially washed and prepared for injection
into the eggs.
 This is accomplished using a microscopic pipette while the
eggs are visualized and held in place by an instrument known as a
micromanipulator. This is a very delicate procedure requiring dexterity and
precision. Our embryologists, have extensive ICSI experience and they
consistently produce high fertilization rates. Normal fertilization is
expected in approximately 70% of the eggs that are injected and the
pregnancy rates are similar to those achieved with routine IVF and are
dependent on female age and other factors. This is accomplished using a microscopic pipette while the
eggs are visualized and held in place by an instrument known as a
micromanipulator. This is a very delicate procedure requiring dexterity and
precision. Our embryologists, have extensive ICSI experience and they
consistently produce high fertilization rates. Normal fertilization is
expected in approximately 70% of the eggs that are injected and the
pregnancy rates are similar to those achieved with routine IVF and are
dependent on female age and other factors.
After the ICSI procedure, the fertilized eggs (embryos) are
placed in incubators where they remain until ready for transfer.
 top
top
Microsurgical Epididymal Sperm Aspiration (MESA)
Testicular
Sperm Extraction (TESE)
These procedures are offered to couples in cases where the
male has no sperm present in the ejaculate. They are used in conjunction
with an ICSI procedure.
In some semen samples there may be no sperm present in the
ejaculate. There can be a variety of reasons for an absence of sperm known
as Azoospermia.
-
There may be a blockage of the tubules that carry the sperm
from the testicles to the penis.
-
The passages themselves may not have developed so sperm
cannot be transported. This is known as absence of the vas
deferens.
-
In some cases sperm may be produced but in low numbers, and
therefore not seen in the semen sample.
-
The male may have had a vasectomy performed which means
that the passages that carry the sperm have been severed.
Testicular Sperm Extraction (TESE)
This procedure may be performed under GA or local anaesthetic
with sedation. A small sample of testicular tissue is extracted from the
testes. This can be achieved by either a fine needle being inserted into the
testes or a small incision being made.
Sperm that is extracted by the above procedures will then be
used in conjunction with an ICSI cycle.
Micro-epididymal Sperm Aspiration:(MESA)
MESA is a procedure to retrieve sperm from the epididymis in
men who have a diagnosed blocked vas deferens It is normally carried out
under general anaesthetic. The sperm that is taken from the epididymis
usually has poor motility so doctors usually proceed to ICSI on the same
day.
 top
top
Sperm
Cryopreservation and Thawing
The process of preserving sperm by means of freezing for use at a later
time.
Sperm can be
cryopreserved in cases where the male might have difficulty in producing a
specimen at a given time. If sperm were retrieved microsurgically, excess
sperm may be stored to avoid having to repeat the invasive surgical
procedure. Also, for patients planning to undergo chemotherapy or
radiotherapy (for cancer), sperm may be cryopreserved as the therapy may
diminish their sperm production. Sperm can also be frozen for persons
wishing to donate their sperm to infertile couples.
Sperm retrieved by masturbation, testicular biopsy or microsurgical
epididymal sperm aspiration are placed together with a cryoprotectant and
stored in cryostraws in liquid nitrogen at a temperature of -196°C. This can
be thawed at any time, and the cryoprotectant can be removed and the sperm
used for ART procedures.
 top top
Embryo Cryopreservation and Thawing
Embryo freezing, called embryo cryopreservation, has helped thousands of
infertile couples have healthy babies since the mid-1980s. The process of
unthawing frozen embryos and implanting them into a women’s uterus is called
frozen embryo transfer (FET). Candidates for this process are:
-
Couples who undergo IVF and have excess embryos they’d like
to use later on. They can have a few more chances at pregnancy without
having to endure another IVF process involving hormone injections,
surgical procedures, numerous doctor’s visits, and emotional and financial
tolls.
-
Couples in which one partner must undergo chemotherapy or
radiation treatment that may destroy their ability to produce healthy eggs
or sperm.
-
Single men and women facing cancer treatment that may
render them infertile. They can preserve their sperm or eggs (gametes) and
use donor gametes to produce embryos to be used after recovery.
The Process
Embryos can be frozen from one to six days after
fertilization. The freezing
process involves mixing the embryos with a solution that prevents ice
crystals from forming between the cells, which can destroy them. The embryos
are then placed in glass viles which are secured in liquid nitrogen freezers
and are cooled slowly to -196° C (-400°F). When needed, the embryos are
thawed, and bathed in solutions to remove the freezing cryoprotectants.
 top top
Sperm Donation
The donation of sperm for the use by infertile couples with severe male
factor infertility.
Indications for using
donor sperm:
Donor sperm may be used when the male partner has azoospermia or severe male
factor, has a know hereditary/genetic disorder that could be carried over to
biologic offspring, or has had previously failed IVF attempts and do not
choose to have ICSI. Donor sperm may also be used in females without male
partners.
 top top
Oocyte Donation
Many women who’ve not been able to conceive but want to experience pregnancy
and childbirth turn to egg donation. Poor egg quality due to a woman’s
advanced age is the most common reason why single women and couples turn to
egg donation.
Egg donation is commonly used by:
-
Couples in which the woman has poor quality or no eggs, but
who want a biological child using the husband’s sperm
-
Women with no ovaries but an intact uterus
-
Women with genetic factors that they don’t want to pass on
to their children
The first known pregnancy achieved with a donated egg
occurred in 1984. Today, an estimated 10,000 babies a year are born
worldwide from donated eggs.
The Process
Eggs, called oocytes, are surgically retrieved from healthy
young women, generally between 21 to 30 years old - at their reproductive
prime and old enough to give informed consent. Egg or oocyte donors undergo
psychological and medical screening, which includes a thorough medical
history and workup. .Next, donors receive hormone injections to induce a
superovulation (five or so eggs versus one, which women naturally release
each month). A doctor then surgically removes eggs from the donor’s ovaries.
The lab will attempt to fertilize several eggs in vitro (in a laboratory)
using the recipient’s partner’s sperm . Fertilized eggs (embryos) are then
inserted into the recipient’s uterus. If successful, the embryo will attach
to the uterine lining and develop into a healthy baby.
 top top
Gender Selection
Gender selection may be used when parents
want a child of a specific sex, a “balanced family”—a boy and a girl, for
example, or in instances where sex-linked diseases such as hemophilia are a
concern. Methods include preimplantation genetic diagnosis (PGD)
Preimplantation Genetic Diagnosis
Preimplantation genetic diagnosis (PGD) involves testing one
cell of 3-day-old embryos that are created via in vitro fertilization (IVF).
One cell from the embryo is removed to analyze its
chromosomal makeup, which indicates whether the embryo is female or male.
Only embryos of the desired sex are transferred to the uterus during the IVF
cycle.
 top top
Surrogacy
Surrogacy or gestational care is
a family building option for those who want a child with genetic ties and
have not had success with other “first-line” assisted reproductive
technology (ART) treatments.
Traditional and Gestational
Two types of surrogacy - traditional and gestational - are
practiced today. In traditional surrogacy, a woman called a “surrogate
mother” carries an embryo conceived with
her own egg and the sperm of a male who, with his partner, wants a baby. In
gestational surrogacy, the surrogate, called a gestational carrier, gives
birth to a baby conceived with an egg and sperm of a couple or a donor egg
or sperm. The majority of surrogates today are gestational carriers.
Traditional surrogacy can be done via intrauterine
insemination
IUI or in vitro fertilization (IVF).
With gestational surrogacy IVF is used to fertilize the eggs in a
laboratory. If the fertilization is successful, a doctor transfers some or
all of the resulting embryos (often 2 or 3) into to the surrogate’s uterus.
If all goes well, the surrogate/gestational carrier delivers the baby and
immediately relinquishes him/her to the parent(s).
Candidates for surrogacy are:
-
Couples and single women who have had multiple
miscarriages, or difficulty conceiving and/or carrying a fetus to term.
Surrogacy enables them to have a child genetically related to one or both.
-
Couples or single women in which the woman has no uterus or
a congenital anomaly of her uterus but has intact ovaries.
What to Consider
Surrogacy involves many legal, ethical and financial
considerations. Usually potential parents pay the surrogate a fee for
carrying the child, along with her medical expenses. Costs can start at
$20,000 or more, up to $120,000. Legal contracts are required before the
process begins to protect the rights and responsibilities of the parents,
surrogate, and intended child. Both the third party and intended parents
should have separate legal counsel.
surrogates already have had a child/children of their own,
are healthy medically and emotionally, and are not motivated solely by
financially considerations.
 top top
President Elias Sarkis Avenue, Saab Bldg, 3rd floor, Sodeco, Beirut-Lebanon
Phone:+961-1-610400, Fax:+961-1-612400, email: info@meivf.com
|

